Chemotherapy With Antisense Oligonucleotide Therapy Improves Disease-Free Survival
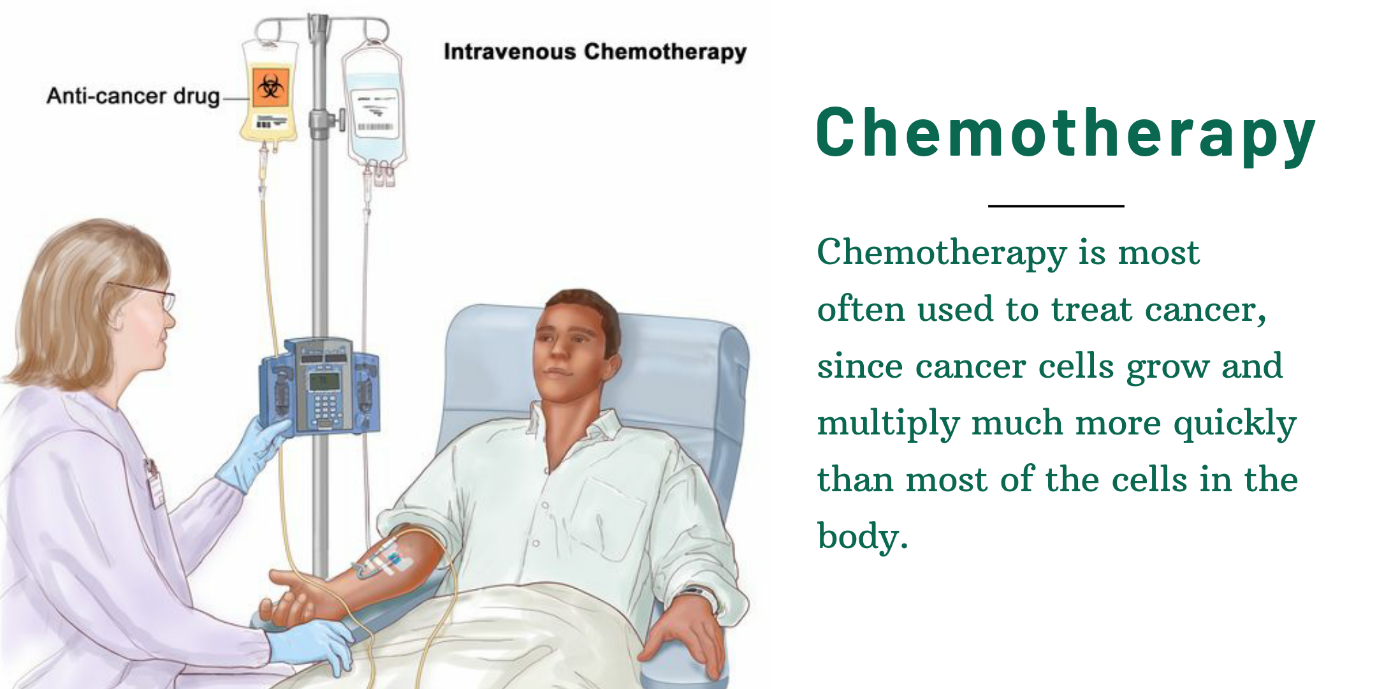
Chemotherapy
Chemotherapy is a cancer treatment that involves the use of medication to eradicate cancer cells. Chemotherapy drugs come in a wide variety of forms, but they all function similarly. They block cancer cells from procreating, which stops them from developing and spreading throughout the body.
Besides cancer, chemotherapy is also used for immune system disorders and several bone marrow diseases. Chemotherapy comes in a variety of forms. Chemotherapy medications, in general, are potent chemicals that kill cancerous cells at times of the cell cycle. The cell cycle is the process through which new cells are created in all living things. Chemotherapy has a greater impact on these rapidly proliferating cells because cancer cells go through this phase more quickly than normal cells [1].
Chemotherapy can harm healthy cells as they go through their natural cell cycle since it circulates throughout the entire body. This explains why chemotherapy side effects including nausea and hair loss might occur.
When is chemotherapy used?
If cancer has spread or there is a chance that it may, chemotherapy may be employed. It may be utilized for:
- curative chemotherapy
- increase the efficacy of other therapies
- decrease the likelihood that cancer may return following radiation or surgery (adjuvant chemotherapy)
- In the absence of a cure, treat symptoms (palliative chemotherapy)
- lower the total number of cancer cells in your body
- reduce the likelihood of cancer spreading
How is it administered?
There are numerous ways to administer chemotherapy. The most typical kinds are:
- Chemotherapy administered intravenously (intravenous chemotherapy) is typically performed in a hospital and entails the administration of medication through a tube inserted into a vein in the hand, arm, or chest.
- Chemotherapy administered orally (oral chemotherapy) typically entails the administration of a course of medication at home with periodic hospital visits.
Other types of chemotherapies which are given to patients are:
- Injected chemotherapy
- Chemotherapy into an artery
- Chemotherapy into the peritoneum
- Topical chemotherapy
Types
More than 100 different medicines are used in chemotherapy for cancer. Even though all chemotherapy medications cause cell death, they target certain cell types at various points in the cell cycle. Combining medications that harm the cancer cell in several ways can improve the efficacy of the treatment.
The primary forms of chemotherapy are listed below:
- Alkylating substances
- Antimetabolites
- antibiotics for tumors
- Anti-topoisomerase agents
- Mitotic blockers
- Animal alkaloids [2]
Disease Free Survival
Disease-free survival refers to the time following a successful treatment during which there are no visible indications of the illness was cured. This idea is frequently applied to the treatment of cancer and other conditions for which there is no permanent remedy.
DFS (disease-free survival) is one of the most challenging oncology objectives. In contrast to progression-free survival in the context of advanced cancer, which describes the interval between treatment and disease progression (or death) in patients who already have detectable cancer in their bodies, DFS describes the interval between treatment and disease recurrence (or death) following curative-intent therapy. This distinction is crucial because treating a patient in the curative setting is blind; adjuvant treatment efficacy can only be evaluated in the distant future based on whether the tumor recurred. In contrast, in the advanced setting, treatment response can be quickly assessed using imaging or tumor markers. Due to this, risk-benefit analyses in the curative context are not always simple, and medicine that only shows an enhanced DFS may not always be in the best interests of patients [3].
Antisense Oligonucleotide
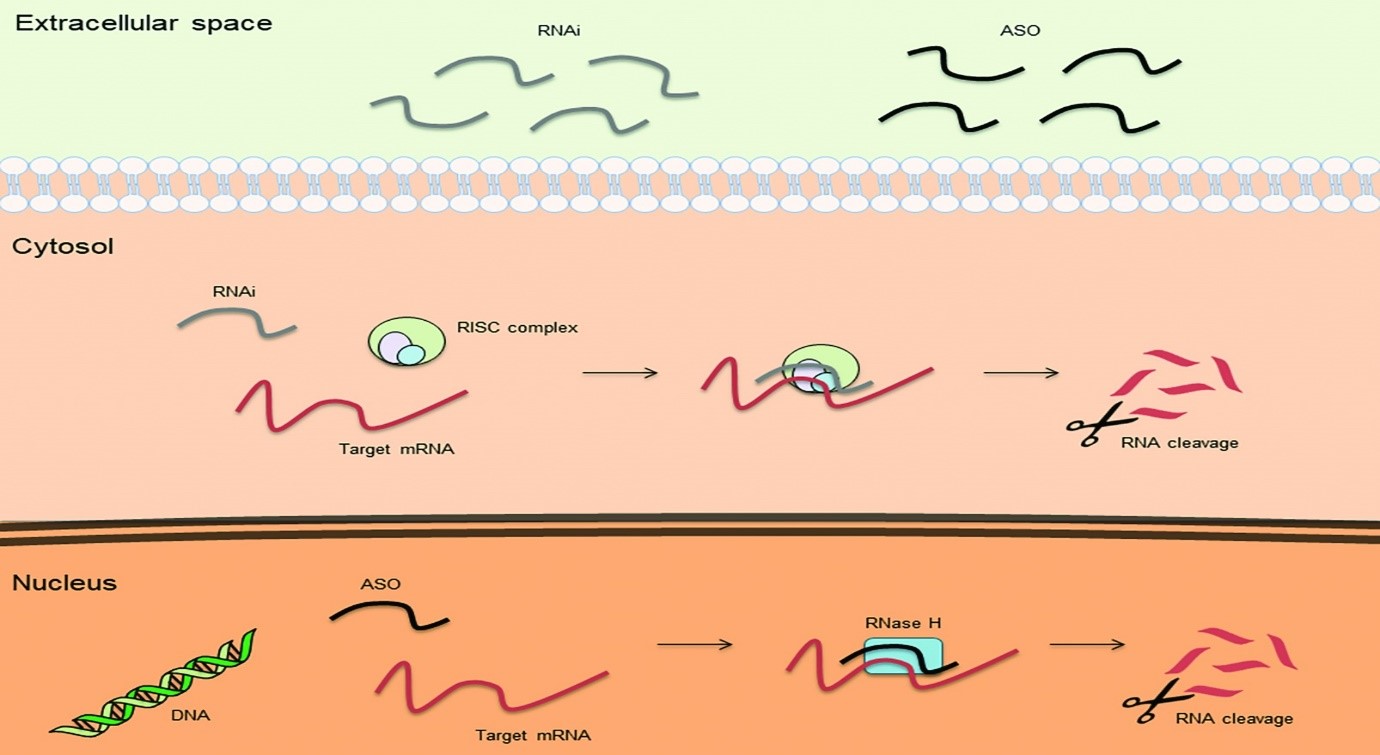
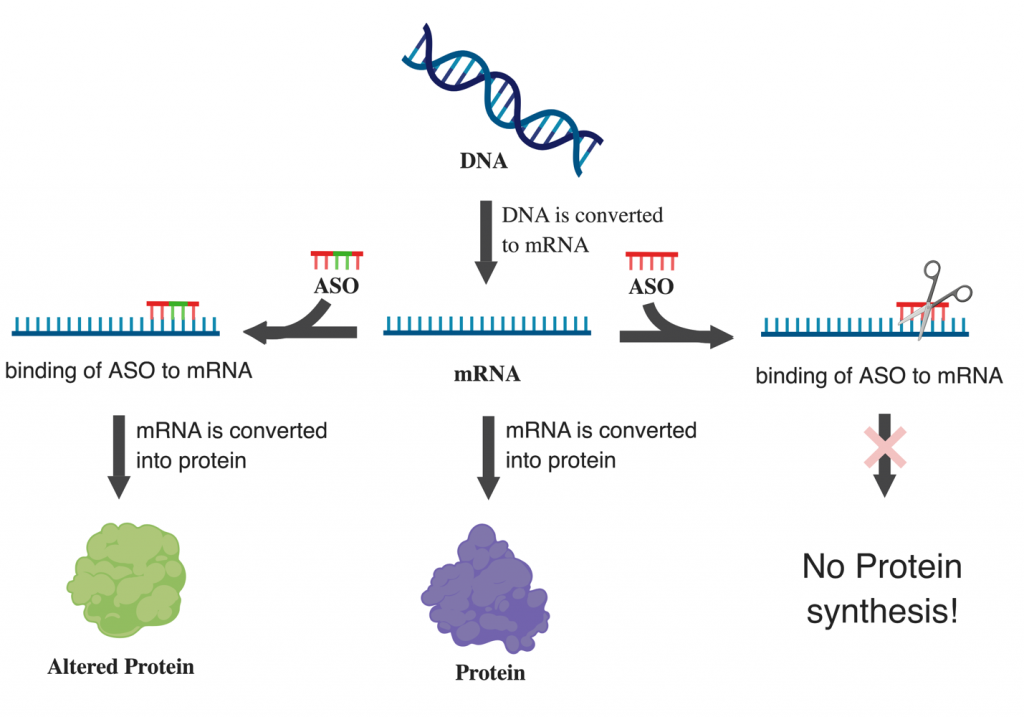
Antisense Oligonucleotides (ASOs), which have been tested in a variety of illnesses, are single-stranded, highly modified synthetic RNA (or DNA) sequences that are intended to bind to the RNA that encodes the desired gene with specificity through complementary base pairing. Synthetic DNA oligomers known as antisense oligonucleotides (ASOs) hybridize to a target RNA in a sequence-specific way. They have been used effectively to silence microRNAs, control messenger RNA splicing, and decrease the expression of genes [4].
How ASOs Work?
Antisense RNAs are essential for controlling gene expression at several stages, including replication, transcription, and translation. Additionally, synthetic antisense RNAs have the power to control the expression of genes associated with the host cell. For the treatment of diseases with a significant inflammatory component, such as arthritis and asthma, lung cancer, diabetes, and ocular damage in AIDS, antisense medicines have been discovered or are “in the pipeline.” Through a variety of unique processes, ASOs can change RNA and decrease, increase, or modify protein expression. ASO-mediated therapies are more likely to be effective since they focus on pathogenesis source [5].
Most ASOs are phosphorothioated because they could be swiftly digested in their “naive” form, reducing their bioavailability. This change makes it easier for ASOs to attach to plasma proteins, which lowers their renal loss and improves absorption into several organs (e.g., liver, bone marrow, and lymph nodes). Because neither RNaseH activity nor ASO solubility is affected by the chemical change, many methods of administration are possible (e.g., subcutaneous, intravenous, topical, oral, or rectal). Toll-like receptors (TLR) can bind to phosphorothioate oligonucleotides with one or more CpG patterns, activating innate immune responses. Choosing oligonucleotides devoid of CG or swapping the C for 5methylC, which does not activate the immune system, can solve this problem.
ASOs have already been employed in several human illnesses. For instance, the FDA authorized the use of fomivirsen in 1998 to treat cytomegalovirus-induced retinitis by preventing the translation of the mRNA encoding for the key immediate early region proteins of the virus. Mipomersen, a drug that targets apolipoprotein B100, was licensed by the FDA in 2013 for the treatment of familial hypercholesterolemia. Subsequently, eteplirsen and nusinersen were launched to treat Duchenne muscular dystrophy and spinal muscular atrophy, respectively. By splicing exon 52 into disease-related exon 51 of the dystrophin RNA, eteplirsen creates a truncated but partially functional protein [6].
Can Chemotherapy with ASOs Improve Disease-Free Survival?
The Spruce trial: Carboplatin and Pemetrexed with Apatorsen (OGX-427)
This randomized, double-blinded, phase II trial evaluated the efficacy of carboplatin and pemetrexed plus either apatorsen, an antisense oligonucleotide targeting heat shock protein 27 mRNA, or placebo in patients with previously untreated metastatic nonsquamous non-small cell lung cancer (NSCLC). The addition of apatorsen to carboplatin and pemetrexed was well tolerated. The primary endpoint was progression-free survival (PFS); secondary endpoints included overall survival (OS), objective response rate, and toxicity. In this small group, patients who received apatorsen had median PFS of 10.8 months, and those who received placebo had median PFS 4.8 months.
Neoadjuvant Chemotherapy with ASOs Success against Luminal Breast Cancer
Neoadjuvant chemotherapy has only modest benefits for patients with luminal breast cancer (LBC). Palbociclib and endocrine therapy have produced remarkable outcomes in advanced LBC. Researchers evaluated letrozole + palbociclib (LP) as neoadjuvant therapy in LBC in a randomized parallel phase II research. The trial comprised postmenopausal women with stage II-III ER-positive HER2-negative breast cancer. Third-generation chemotherapy was administered to the patients (FEC100 x 3 – docetaxel 100 x 3). The findings showed that neoadjuvant LP had a better safety profile than chemo and resulted in a little lower pCR/RCB 0-I rate than chemo. However, clinical response and BCS rates were comparable in both arms. There have been extensive analyses [8].
BCL2 ASOs with Chemotherapy improves Small-cell Lung Cancer
Small-cell lung cancer (SCLC) that is chemoresistant is described as progressing during initial treatment or within three months after that treatment’s end. The prognosis for patients with chemorefractory SCLC is quite bad, and no treatment has been proven to provide meaningful clinical advantages. Most SCLCs have elevated Bcl-2 expression, which has been linked to treatment resistance. Cytotoxic therapy may be more effective against tumors if Bcl-2 levels are reduced by using G3139, an antisense oligonucleotide complementary to the mRNA encoding Bcl-2. In this pilot study of paclitaxel coupled with G3139, twelve patients with chemorefractory SCLC took part. A fixed dose of 3 mg/kg/day of G3139 was continuously infused intravenously over 7 days. On day 6, the dose of paclitaxel was initially 175 mg/m2, but it was lowered to 150 mg/m2 because two of the three patients treated in the first dose cohort had myelosuppression. It was determined that paclitaxel at 150 mg/m2 and G3139 at 3 mg/kg/day were a workable and well-tolerated combination. No unbiased reactions were seen. The greatest plasma G3139 levels were identified in the patient with a long-term stable illness, indicating that individual differences in the metabolism and elimination of the antisense oligonucleotide may affect activity. This study shows that G3139 and paclitaxel can be coupled in a dose range that is cytotoxic, and it is recommended that a similar combination be evaluated for efficacy in the setting of chemoresponsive illness [9].
Olaparib and BCL2 ASOs as an effective Approach against PARP
Human tumor heterogeneity increases the risk of cell subpopulations that are resistant to treatment, which promotes therapeutic failure. Olaparib, a PARP-1 inhibitor, is approved for use in ovarian tumors with BRCA mutations, but BRCA2-reversion mutations result in HRR that is functional and olaparib resistant. Researchers created an antisense technique to make most tumor cells in a population BRCA2-deficient. This allowed them to overcome that resistance and extend the use of PARP1 inhibition to tumors with functional HRR. They state that BRCA2 downregulation boosted olaparib sensitivity in several human tumor cell lines (but not in non-cancer human kidney cells) and increased aneuploidy and chromosomal translocations in human tumor cells when paired with olaparib. Olaparib monotherapy allowed the expansion of HRR-proficient cells resistant to subsequent olaparib treatment in a mixed population of HRR-proficient and HRR-deficient cells. Combining BRCA2 inhibition with olaparib therapy prevented the selection of cells with HRR propensity and restricted population-wide cell division. More effectively than either treatment alone, BRCA2 siRNA and olaparib treatment reduced ovarian xenograft development in mice. Expanding the clinical usage of olaparib and preventing resistance may be possible with the use of BRCA2 antisense oligonucleotides in vivo [10].
ASOs with Chemotherapy against Prostate Cancer
Prostate cancer is genetically caused by the ERG oncogene, a gene that codes for a transcription factor and is a member of the ETS family. In 50% of instances, it is triggered by fusion with the androgen responsive TMPRSS2 promoter. Therefore, there is a lot of interest in creating innovative therapeutics that specifically target ERG. Researchers used an antisense strategy to create morpholino-based oligonucleotides that target ERG by causing the exon 4 constitutive to be skipped. They have created splice-switching oligonucleotides (SSOs), and antisense morpholino oligonucleotides that specifically target the 5′ and 3′ splice sites of exon 4 of the ERG gene. To induce exon 4 skipping in two ERG-positive cell lines, VCaP prostate cancer cells and MG63 osteosarcoma cells, they evaluated their effectiveness. They developed and evaluated morpholino-based SSOs that significantly lower ERG expression, which lowers migratory phenotype, decreases cell proliferation, and increases apoptosis. SSOs have shown promise for oncogene targeting in vivo in preliminary studies using mouse xenografts and a specimen from radical prostatectomy for prostate cancer in a person. This study thus promotes additional in vivo therapeutic trials with SSOs that target the ERG oncogene [11].
References
[1]. DeVita VT, Chu E. A history of cancer chemotherapy. Cancer Res. 2008 Nov 01;68(21):8643-53.
Link: https://pubmed.ncbi.nlm.nih.gov/18974103/
[2]. Chidharla A, Kanderi T, Kasi A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jan 30, 2022. Chemotherapy Acral Erythema.
Link: https://pubmed.ncbi.nlm.nih.gov/29083584/
[3]. Edward L. Korn, Boris Freidlin, in Abeloff’s Clinical Oncology (Sixth Edition), 2020
https://doi.org/10.1016/B978-0-323-47674-4.00018-9
Link: https://www.sciencedirect.com/science/article/pii/B9780323476744000189
[4]. Bennett C.F., Baker B.F., Pham N., Swayze E., Geary R.S. Pharmacology of Antisense Drugs. Annu. Rev. Pharmacol. Toxicol. 2017; 57:81–105. doi: 10.1146/annurev-pharmtox-010716-104846.
https://doi.org/10.1146/annurev-pharmtox-010716-104846
Link: https://www.annualreviews.org/doi/abs/10.1146/annurev-pharmtox-010716-104846
[5]. Stein, C. A. (2001). The experimental use of antisense oligonucleotides: a guide for the perplexed. J. Clin. Invest. 108, 641–644. doi: 10.1172/JCI13885
Link: https://www.jci.org/articles/view/13885
[6]. Khorkova, O., and Wahlestedt, C. (2017). Oligonucleotide therapies for disorders of the nervous system. Nat. Biotechnol. 35, 249–263. doi: 10.1038/nbt.3784
Link: https://www.nature.com/articles/nbt.3784
[7]. Schmid, P., et al. “A phase II, randomised, open-label study of gemcitabine/carboplatin first-line chemotherapy in combination with or without the antisense oligonucleotide apatorsen (OGX-427) in advanced squamous cell lung cancers.” Annals of Oncology 28 (2017): v638.
Link: https://oncologypro.esmo.org/meeting-resources/esmo-2017-congress/a-phase-ii-randomised-open-label-study-of-gemcitabine-carboplatin-first-line-chemotherapy-in-combination-with-or-without-the-antisense-oligonucle
[8]. Palboci Cottu, P., et al. “Letrozole and palbociclib versus 3rd generation chemotherapy as neoadjuvant treatment of minal breast cancer. Results of the UNICANCER-eoPAL study.” Annals of Oncology 28 (2017): v605.
Link: https://www.annalsofoncology.org/article/S0923-7534(20)39100-6/fulltext
[9]. Rudin, C. M., et al. “A pilot trial of G3139, a bcl-2 antisense oligonucleotide, and paclitaxel in patients with chemorefractory small-cell lung cancer.” Annals of oncology 13.4 (2002): 539-545.
Link: https://www.sciencedirect.com/science/article/pii/S0923753419618867
[10]. Rytelewski, Mateusz, et al. “Reciprocal positive selection for weakness-preventing olaparib resistance by inhibiting BRCA2.” Oncotarget 7.15 (2016): 20825.
Link: https://pubmed.ncbi.nlm.nih.gov/26959114/
[11]. Li, L., Hobson, L., Perry, L. et al. Targeting the ERG oncogene with splice-switching oligonucleotides as a novel therapeutic strategy in prostate cancer. Br J Cancer 123, 1024–1032 (2020). https://doi.org/10.1038/s41416-020-0951-2
Link: https://www.nature.com/articles/s41416-020-0951-2
