
Myeloproliferative neoplasms (MPN), previously called myeloproliferative disorders, are diseases of the bone marrow and blood. They can strike at any age, have no known cause, and present with a wide range of symptoms and outlooks.
Sometimes, the disease progresses slowly and requires little treatment; at other times, it develops into acute myeloid leukemia (AML).
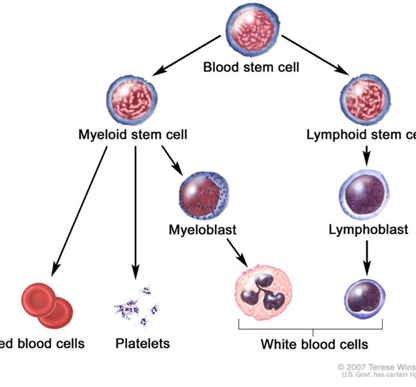
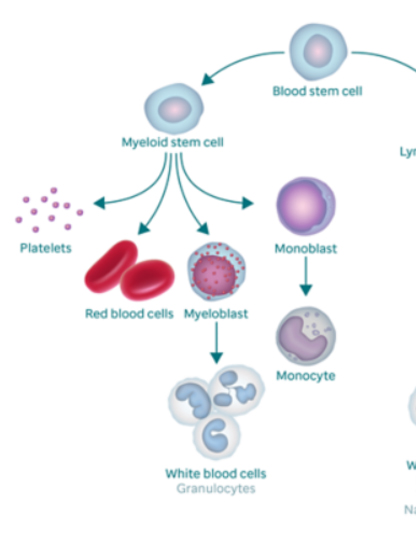
To understand what happens to your blood when you have MPN, it helps to know what makes up normal blood. There are three major types of blood cells; red blood cells (RBCs), white blood cells (WBCs), and platelets.
Red blood cells (RBCs), the major part of your blood, carry oxygen and carbon dioxide throughout your body. The percentage of RBCs in the blood is called hematocrit. The part of the RBCs that carries oxygen is a protein called hemoglobin. All body tissues need oxygen to work properly.
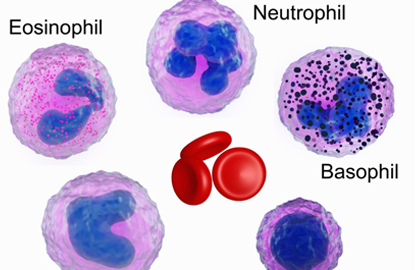
White blood cells (WBCs) include several different types. Each has its own role in protecting the body from germs. The three major types are neutrophils, monocytes, and lymphocytes.
- Neutrophils (also known as granulocytes or polys) destroy most bacteria.
- Monocytes destroy germs such as tuberculosis.
- Lymphocytes are responsible for destroying viruses and for overall management of the immune system. When lymphocytes see foreign material, they increase the body’s resistance to infection.
Myeloproliferative neoplasm types
There are several types of myeloproliferative neoplasms. The main types are:

Myeloproliferative Neoplasm Risk Factors
Anything that increases your chance of getting myeloproliferative neoplasms is a risk factor. These include exposure to:
- Intense radiation, such as a nuclear bomb
- Petrochemicals, such as benzene or toluene
- Electrical wiring
Many people with myeloproliferative neoplasms have a mutation in the JAK2 gene.

Myeloproliferative Neoplasm Symptoms
Often, especially in the early stages, the symptoms of myeloproliferative neoplasms differ from person to person. If you have symptoms, they may include:
- Headache
- Fatigue
- Shortness of breath
- Easy bruising or bleeding
- Petechiae (tiny red spots under the skin)
- Unexplained weight loss
- Night sweats
- Fever
- Pruritus (itching)
These symptoms do not always mean you have myeloproliferative neoplasm. However, it is important to discuss any symptoms with your doctor, since they may signal other health problems.
Myeloproliferative Neoplasm Diagnosis
At ART OF HEALING CANCE, we have extensive expertise in diagnosing myeloproliferative neoplasms, as well as the latest technology to do so. Our hematopathologists specialize in myeloproliferative neoplasms, giving them the knowledge to pinpoint your exact diagnosis.
Diagnosis of myeloproliferative neoplasms can be challenging. It often does not have symptoms in the early stages, and when it does they are often mistaken for signs of other diseases. A doctor must have a high degree of experience in myeloproliferative neoplasms (MPN) to make an accurate diagnosis.
If MPN is suspected, blood tests will be ordered. The blood test results can validate the suspicion, but a bone marrow biopsy may be required to definitively confirm the diagnosis.

Myeloproliferative Neoplasm Treatment
ART OF HEALING CANCER has a level of experience and expertise that can make a profound difference in your treatment.
The three classic MPN subtypes are myelofibrosis, the most aggressive MPN; polycythemia vera, the most common; and essential thrombocythemia, the most indolent.
Myeloproliferative neoplasms can be challenging to treat. Patients may require years of therapy and follow-up care. Treatments for MPN are generally aimed at controlling disease symptoms, and your symptoms will help the doctor decide which treatment is best. Therapies may include one or more of the following:
- Medications: aspirin, hydroxyurea, anagrelide and interferon-alpha are the main medications for essential thrombocythemia and polycythemia vera. Ruxolitinib can be used in polycythemia vera patients not responding to hydroxyurea. Ropeginterferon alpha-2b was approved as a first-line treatment for PV in the United States in November 2021. For myelofibrosis, ruxolitinib and fedratinib (JAK inhibitors) are approved therapies. Thalidomide, steroids and other hormones, and cladribine may also be used. Pacritinib received accelerated regulatory approval for patients with myelofibrosis and very low platelet counts (thrombocytopenia) in February 2022.
- Blood or platelet transfusion
- Growth factors, which stimulate growth of bone marrow cells, are given as injections under the skin and may benefit myelofibrosis patients with low blood cell counts.
- Radiation therapyof the spleen in patients with myelofibrosis
- Surgicalremoval of the spleen in patients with myelofibrosis
- Phlebotomy for patients with polycythemia vera
- Stem cell transplantin patients with myelofibrosis